The HOPE Hand.
What are you doing right now other than scrolling through this article? Do you have a cup of coffee in one hand, your phone in the other? Maybe your right hand is using your laptop mouse and your left hand is holding a snack. Have you ever thought about how often we are using both of our hands? Having two healthy human hands allows us to carry too many grocery bags in one hand and unlock our apartment door with the other, and perform complex bimanual coordination like playing Moonlight Sonata by Beethoven on the piano (well, maybe not all of us can do that). Having two hands also allows us to do some of the most simple tasks in our daily lives, like holding a jar of peanut butter and unscrewing the lid, or putting our hair up in a ponytail.
If you take some time to think about how often both of your hands are occupied, you might start to realize that life could be challenging if you were missing the functionality of one or both of your most useful end effectors (as we call them in robotics). This thought experiment is the reality for someone like my friend Clare, who got into a car accident when she was 19. The impact of the crash resulted in a traumatic brain injury (TBI) that left the right side of her body partially paralyzed. In addition to re-learning how to walk, she also had to learn how to navigate her life with one functioning hand.
To get a better idea of what that would be like Clare says, “Tie your dominant hand behind your back. Try it!”
There are other neurological conditions, in addition to TBI, that could result in paralysis: stroke, spinal cord injury, cerebral palsy. When we hear the word paralysis, partial paralysis, or hemiparesis (partial paralysis of one side of the body), we might envision someone’s limb being weak and hanging at their side. This manifestation of motor impairment is only the case for a fraction of the hemiparetic population. For others like Clare, their hand and elbow are reflexively kept in a flexed position, or flexor synergy pattern, meaning that their hand is tightly closed in a fist, regardless if they try to open their hand or close it. They have little to no ability to voluntarily extend their fingers, and the amount of muscle force keeping the hand closed changes from moment to moment. If we think back to the peanut butter jar example, imagine having to use your able hand to pry open the fingers of your impaired hand to get them around the jar of peanut butter.
Thankfully, there are occupational therapists that can train individuals to adapt their approaches to activities of daily living, and physical therapists that keep their hands and limbs stretched and mobile. But also, the robotics community has been working on their own technology-based contributions to the recovery and long-term independence of individuals with hand impairments due to neurological injury. There are decades of research in the field of wearable assistive and rehabilitation devices, creating new prosthetics and exoskeletons to help individuals overcome their physical impairments. However, we came across a gap in the research when we began working with Clare and other individuals with similar hand impairments.
Most of the assistive hand exoskeletons currently being developed or commercially sold focus on restoring the user’s ability to grasp with their impaired hand. However, Clare actually needed an exoskeletal device that extended her fingers, against varying levels of resistance due to increased resting muscle tone or spasticity (click here to read about our finger extension force study). As a result, we developed the HOPE hand, a hand orthosis with powered extension to better serve individuals like Clare who need assistance opening their hand, to provide them with improved capabilities to perform activities of daily living, and to help them re-gain their independence.
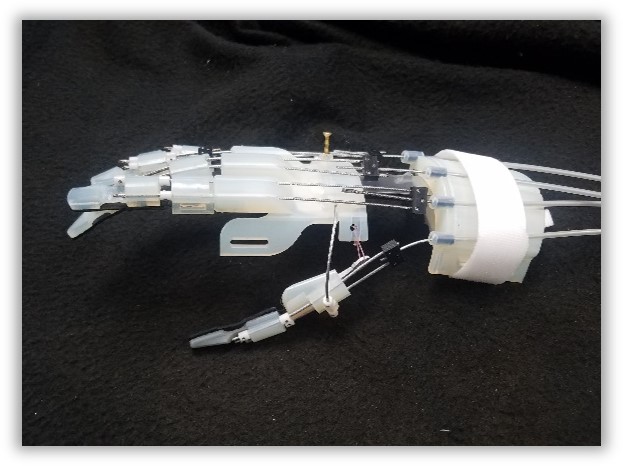
The HOPE Hand is a cable-driven hand exoskeleton that uses pushing and pulling forces along the back of the hand to open and close the fingers individually. Each finger has two cables running parallel along the back of the finger which prevents medial/lateral movement and stabilizes the joint at the base of the finger. The cables are guided by rigid links that are attached to the finger using medical tape, and connect to a worm gear driven by a DC motor. The index finger and middle finger are actuated individually, and the pinky and ring finger are coupled, so they move together. The thumb has two degrees of freedom; flexion and extension are performed similarly to the other fingers, and abduction/adduction (to move the thumb into a position across from the fingers for a power grasp), is positioned manually by the user. This mechanical design allows the user to perform functional grasps by overcoming the increased muscle tone in their hand.
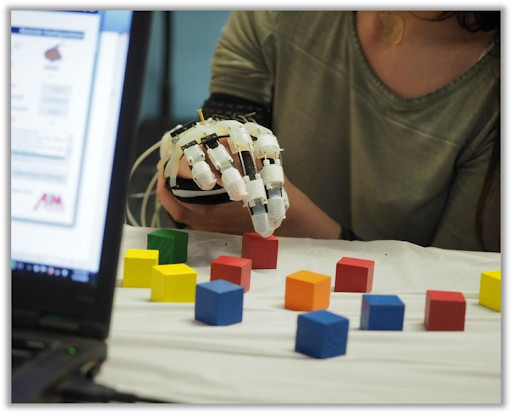
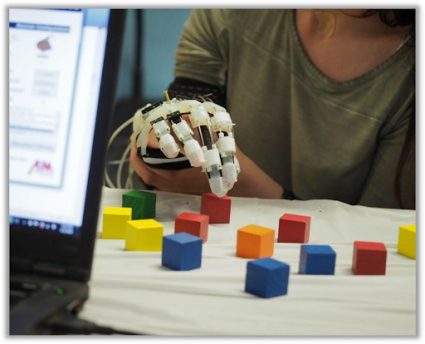
When we asked Clare to test out the HOPE Hand, she was happy to contribute to the research! She was able to pick up and move colored blocks from one designated area to another with the HOPE Hand, compared to not being able to pick up any blocks without the assistive device. We continued to work with Clare, her mom, and her physical therapist throughout our iterative device development process so she could give feedback and we could improve the device. We found that involving end users like Clare from the beginning was critical to designing a device which is safe, comfortable, and most importantly, usable. It was also the best way for us to understand her daily challenges and the nature of her hand impairment.
Clare’s physical therapist says “It engages the patient’s brain in ways that she would not be exposed to without participating in research, which could forge new neural pathways. I can watch the way she reacts and responds to the new technology and that enables me to create different rehab strategies to enhance recovery.”
While the HOPE Hand isn’t quite available to consumers yet, our collaborative team of patients, clinicians, caregivers, and academic researchers is making progress. One of the current challenges we are tackling, along with the rest of the wearable device industry, is how the device recognizes the user’s intention to move. The majority of electric prostheses and hand exoskeletons use residual muscle activity (myoelectric control) as an indicator of intention to move. However, the unreliable muscle activity that can be present due to neurological conditions like traumatic brain injury, can make this form of control challenging. Because of this, researchers are diving into alternative control methods such as computer vision and brain activity. We have implemented a voice control alternative, which also gives users an opportunity to practice their speech, as it is common for conditions like stroke and TBI to result in speech impairments such as aphasia, in addition to motor impairments. It has been valuable for us to consider the complexities of our targeted users, to create a device that could potentially help in more ways than one.
They say many hands make light work, but let’s start by restoring the functionality of the original two, so Clare can open that jar of peanut butter as fast as you can click on the next article while sipping your morning coffee.
tags: c-Health-Medicine

Tess Meier
is a PhD candidate in robotics engineering at Worcester Polytechnic Insitute in Worcester, Massachusetts.

Tess Meier
is a PhD candidate in robotics engineering at Worcester Polytechnic Insitute in Worcester, Massachusetts.
Credit: Source link

Comments are closed.